Abstract
Introduction: The prevalence of sickle cell disease (SCD) is higher in Blacks, with variable disease prevalence in various regions. However, studies comparing outcomes in the different ethnic backgrounds are not widely available. Therefore, we examined the disparities in disease complication hospital-related outcomes among racial groups in SCD.
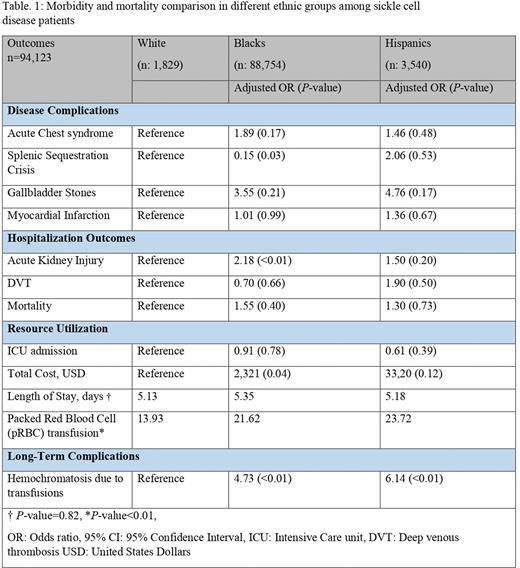
Methods: We investigated the National Inpatient Sample 2019 employing International Classification of Diseases-10 (ICD-10) codes to include adult SCD patients. Morbidity, disease complication, and resource utilization were compared, stratified by racial groups, with White as the reference group. Analyses were performed using STATA (version 14.2), considering 2-sided P< 0.05 as statistically significant. Proportions were compared using Fisher exact test and continuous variables using the Student's t-test. Confounding variables were adjusted using multivariate logistic and linear regression analyses and included: gender, Charlson Comorbidity Index, median household income for patients' zip codes, hospital location/region/bedside, and insurance status.
Results: A total of 94,123 patients were included (mean age 34.61 years, 94.29% Black, 3.77% Hispanics, and 1.94% Whites). All racial subgroups had similar odds of disease complications from SCD except for splenic sequestration crisis (85% higher odds in Whites; Adjusted odds ratio (aOR) 0.15, P=0.03). Higher odds of acute kidney injury were observed in Blacks (aOR 2.18, P<0.01). The length of stay was similar among racial groups; however, blacks incurred higher hospital costs. Blacks and Hispanics required more blood transfusions during hospital stray. On retrospective analysis of ICD-10 codes, there were more cases of secondary hemochromatosis due to iron overload in Blacks and Hispanics.
Discussion: Racial disparities exist in the disease complication and hospitalization outcomes in SCD patients. Blacks and Hispanics are also at risk of secondary hemochromatosis. Further research is required to establish specific causes.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal